Healthcare facilities are constantly searching for ways to improve the efficiency of their operations. To do this, they use various metrics to help them measure and analyze their performance and take action when needed.
Hours per patient day (HPPD) is a pivotal metric for facilities in the following ways:
- Analyzing their nursing workforce
- Predicting patient census fluctuations
- Informing operations budgeting
- Assessing unit staffing needs
- Improving staffing efficiency
What is HPPD in healthcare?
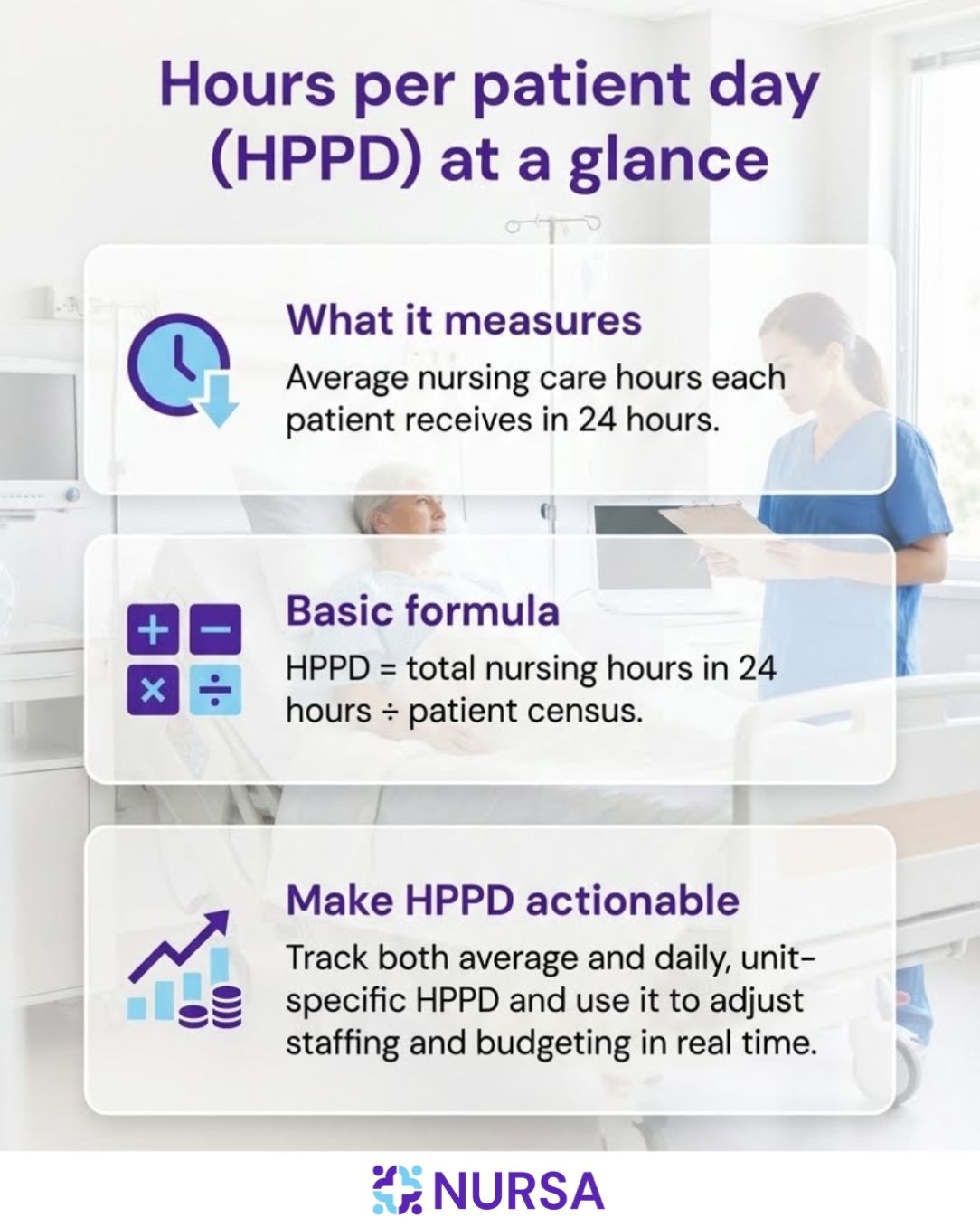
Hours per patient day (HPPD) measures the average number of hours of care every patient receives from nursing staff each day. HPPD is often used to monitor staffing levels, enabling facilities to maintain or adjust nurse-patient ratios to deliver high-quality care.
HPPD does not include paid sick time, vacation, education leave, etc., only the actual hours worked by nurses at the facility that day, divided by the patient census.
Pro-tip: Hours per patient day is also commonly referred to as "hours per resident day" (HPRD) when used in assisted living facilities and other long-term care settings.
How to calculate HPPD
Some medical facilities calculate patient census once a day to measure the average daily census (ADC), while others calculate it hourly to collect more precise figures. HPPD can be calculated for specific days or as an average for a season, month, or another period of time.
Calculating the HPPD requires adding the total number of nursing hours worked in 24 hours and then dividing it by the patient census during that time period.
HPPD = Nursing hours worked in 24 hours / patient census
Terms to clarify:
- Nursing hours: The sum of all hours spent by nursing personnel—including registered nurses, licensed practical nurses, and aides—providing care within a 24-hour period.
- Patient census or patient days: The total number of patients for the same 24-hour period.
Once you have the ADC plus acuity data, staffing grids are often used to determine the target HPPD and inform budgeting. The staffing grid is a dynamic management tool used to translate the required nursing workload into the actual number of staff needed for a specific unit on a particular shift.
Averages vs specific daily HPPD? Which is more useful?
Neither is better—they simply serve different purposes.
Average HPPD helps to inform seasonal comparisons and reliably set tracking goals. It should be used to track performance trends, set budgets, and do long-term planning.
Daily HPPD shows the real-time picture. It helps managers and schedulers spot a shortage or surplus in nurses and take appropriate action. It helps facility managers assess staffing for an unusual day and take immediate action.
Think of it like a weather forecast: You look at the monthly average temperature for packing, but you check the specific daily temperature to decide on today's outfit.
Is there an optimal number of nursing hours per patient day?
There is no single optimal or “perfect” number of hours per patient day for all healthcare facilities. Because different settings provide different types of care, they have varying levels of need for nursing care. Several patient acuity and nurse workload factors affect the ideal HPPD for your facility or unit.
Patient acuity factors:
- Level of instability in the patient’s condition
- Complexity and frequency of required nursing interventions
- Patients’ level of dependency
Nurse workload factors:
- Admissions/discharges/transfers within the shift
- Patient or family education
- Mentoring nursing students
- Time-consuming interventions such as wound and ostomy care and patient incontinence
- Patient safety concerns, such as fall risk
- Sensory and communication difficulties (vision, hearing, non-English speaking)
- Highly agitated or confused patients or the use of restraints
However, averages and benchmarks help guide the use of HPPD in planning, budgeting, and scheduling.
Average HPPD by type of facility or unit
Average HPPD varies significantly between hospital units, showing that higher patient acuity levels require higher HPPD. Unit averages are as follows:
- ICUs: 16.2
- General acute-care units: 8.8
- Step-down units: 8.3
- Labor & delivery: 8.2
- In-patient rehabilitation: 8.1
- Medical-surgical units: 7.2
- Nursing homes: 3.7
CMS payroll-based journal data shows a range from 3.1 nursing hours per patient day in rural for-profit nursing homes to 4.1 in non-rural, nonprofit homes.
The formula for how to calculate HPPD is the same for nursing homes, hospitals, or other facilities, although the number of nurse staffing hours per patient varies.
Long-term care has a more stable patient census and a general need for minimum daily staffing hours with a strong focus on consistent, ongoing care. In contrast, acute care facilities tailor staffing to meet variable patient acuity and rapid care needs.
Compliance and regulatory factors
The CMS 2024 federal nursing home staffing mandate required 3.48 nursing hours per patient day.
However, in July 2025, the One Big Beautiful Bill Act imposed a moratorium on this HPPD regulation, prohibiting its enforcement until October 1, 2034.
Currently, there are no federal regulations currently mandating a specific HPPD figure by facility type. However, as of 2025, some states regulate nurse staffing, primarily through mandated staffing committees, public reporting, or specific HPPD requirements.
States with the strictest HPPD or ratio mandates
California, Florida, Massachusetts, New York, and Rhode Island have the highest mandated minimum HPPD requirements for nursing homes, ranging from 3.5 to 3.81 hours. Compliance remains a challenge, even in California, where these requirements were established over 15 years ago.
California is the only state with mandated minimum nurse-to-patient ratios across all hospital units and specialties. These are not specifically HPPD, but a direct ratio mandate that has a similar effect on staffing levels.
Because California also tracks direct care hours closely for regulatory compliance, HPPD documentation becomes tightly linked to ratio enforcement and daily staffing accuracy.
As such, California facility managers use the CDPH 530 Form to have complete and accurate HPPD. Independent contractor nurses and in-house staff must complete the CDPH 530 form for every shift where they provide direct nursing care. Facilities add these hours to the hours of direct care that other permanent staff provide.
Connecticut, Illinois, Nevada, and Washington, D.C. also have regulations addressing nurse staffing, which may include HPPD considerations.
Why should facilities track the HPPD?
Tracking HPPD is fundamental to healthcare to address crucial administrative issues, such as the following:
- Maximize performance: HPPD can help facilities improve workforce management by informing the analysis of unit nurse staffing levels.
- Increase cost efficiency: HPPD helps identify nursing requirements per unit, project budgets, and increase control over operational costs.
- Improve the quality of patient care: Adequate staffing levels improve the patient experience and outcomes. Monitoring HPPD can help healthcare providers identify the right balance between efficient staffing and high-quality patient care.
- Comply with regulations: Government or state regulations may require facilities to meet HPPD staffing levels or nurse-patient ratios. Staffing ratios directly impact HPPD.
How to manage your facility’s nursing HPPD
To effectively manage your HPPD, you need a baseline to compare with benchmarks and adjust your planning and strategies.
1. Establish a baseline HPPD
Facilities need an accurate picture of where they stand before experimenting with their optimal HPPD.
A baseline HPPD audit converts abstract concepts into actionable metrics by identifying exactly where and how nursing time is being spent.
1a. Collect data for at least one full reporting cycle
Gather data over a period long enough to be statistically representative.
- Recommended cycle: Typically one fiscal quarter (13 weeks), but a minimum of 30 days.
- Source for the number of nursing hours: Payroll or time-and-attendance data from your financial system.
- For the total number of patient days: Patient census data from your patient administration system.
1b. Calculate your current HPPD (total and by unit)
The calculation provides the average hours of direct nursing care a patient receives each 24 hours.
- Total facility HPPD: Use the aggregate numbers for the entire hospital or facility.
- Unit-Specific HPPD: Perform the calculation for every individual unit. This is critical because patient acuity varies dramatically, making a single hospital-wide number almost useless for making local staffing decisions. Unit-specific HPPD is the true baseline.
1c. Compare against nursing per patient day benchmarks
Comparing your actual HPPD to established benchmarks tells you if your staffing level is an outlier (too high or too low) and helps set suitable future targets.
- Internal benchmarks: Compare the unit's current HPPD to its budgeted HPPD and its own historical HPPD (from the previous year). This highlights local efficiency trends.
- External benchmarks (standard ranges): Compare only to units of similar patient acuity and type.
- Strategic benchmarking: You may also compare with peer organizations to determine a competitive range.
2. Adjust HPPD to meet patient care needs
Each facility or unit focuses on caring for patients with different healthcare needs. Understanding their patients’ needs can help facilities plan for the appropriate staffing levels. Appropriate staffing levels lead to optimal HPPD.
Facilities need procedures that allow them to have more control over staff utilization to provide the proper care. The HPPD metric allows facilities to examine how they are using their workforce and identify where to make adjustments.
3. Take note of staffing mix and overtime hour trends
HPPD is typically used with other metrics to analyze staffing levels and hidden costs.
Skill mix analysis: Calculate the percentage of total productive hours contributed by each personnel type—registered nurses (RNs), licensed practical/vocational nurses (LPNs/LVNs), and unlicensed assistive personnel (UAPs)—to understand your staffing model.
This is often expressed as the percentage of RNs out of the total direct care nursing staff.
For example, a unit with 60% RNs, 20% LPNs, and 20% UAPs has an RN skill mix of 60%.
Note: A lower RN percentage (RN-HPPD) may indicate a cost-saving approach, but be cautious about that thought; research links it to poorer patient outcomes.
Overtime (OT): Track the percentage of total hours that are overtime. High OT is expensive and signals a failure in scheduling or a chronic staffing shortage, leading to nurse fatigue and burnout.
Related: Learn the top ways healthcare providers can reduce their reliance on overtime.
4. Adjust your staffing and scheduling strategies
The HPPD analysis directly informs changes, moving the process from evaluation to improvement.
- An actual HPPD below the expected minimum suggests a high risk of adverse patient outcomes. You may need to consider immediate hiring or adjusting your scheduling strategies.
- An HPPD above the expected range might be a sign of inefficiency and indicate a need to implement scalable staffing.
That said, some situations merit a higher HPPD, such as higher-than-expected patient acuity.
5. Monitor and adjust continuously
HPPD is only useful if it drives real-time action. Tracking this metric daily (not monthly or quarterly) helps facilities identify when staffing levels no longer match patient needs and adjust before quality or costs drift off target.
Examples of actionable adjustments include:
- Reassigning clinicians between units when acuity surges in one service line but drops in another.
- Posting short-notice PRN shifts when census spikes unexpectedly rather than staffing up permanent labor prematurely.
- Flexing down scheduled staff the following day when the prior 48 hours trend toward lower patient volume.
- Adjusting staff mix (RN/LPN/CNA ratio) based on the complexity of the current patient population.
- Rebalancing shifts (day vs night) if resource demand trends consistently skew toward certain hours.
Continuous monitoring allows facilities to pivot in real time, keeping staffing safe, efficient, and aligned with actual workload instead of static assumptions.
6. Prepare for higher patient volumes
HPPD is a powerful planning metric that helps forecast seasonal care demand, anticipate operational budgets, and model staffing needs in a way that reduces burnout risk and turnover exposure.
Based on seasonal census trends at your facility, how does your approach to staffing change throughout the year? Some facilities find cost savings by keeping the nursing team staffed to max capacity, or staff for 80-90% facility capacity and using contingent staffing solutions to more efficiently staff for surges.
7. Automate HPPD tracking with technology
Healthcare technology—including EHRs, telehealth, and staff management platforms—can automate workflows to improve productivity and maintain accurate hours per patient day tracking.
Because these systems now directly support HPPD monitoring and staffing decisions, cybersecurity is no longer just an IT concern but a patient safety and workforce risk management priority.
Protecting these tools ensures data integrity remains intact when facilities need to make fast census-based adjustments. Keep your facility safe by implementing these tips to boost cybersecurity.
How PRN staffing helps facilities optimize HPPD
Fluctuations in census can strain operational budgets and make consistent staffing difficult. Using on-demand PRN clinicians can help facilities maintain targeted HPPD ranges during seasonal variation or unexpected surges—without committing to unnecessary fixed labor costs year-round.
For example: With Nursa, facility administrators can post PRN shifts to easily keep staffing levels in alignment with actual patient volume. This approach gives facility leaders a scalable option for filling gaps rapidly while avoiding chronic overstaffing or understaffing. In addition, this also helps reduce the administrative lag time associated with traditional full-time recruitment cycles.
When used responsibly and aligned with acuity-based staffing models, flexible on-demand labor can support safe staffing ratios, protect budget integrity, and reinforce patient care quality. The key is using PRN strategically—not as a default replacement for core staff, but as an intentional tool to right-size staffing in real time.
With that foundation set, the next step is optimizing HPPD through intentional implementation and ongoing measurement.
Leveraging PRN options to strengthen HPPD performance
Platforms like Nursa enable facilities to flex staffing in real time by accessing credentialed per diem nurses as census fluctuations occur. This approach supports safer HPPD performance while helping control labor costs.
Need help reaching your optimal HPPD? Post your open shifts on Nursa to find high-quality per diem talent.
Sources:
- Optimal scheduling and staffing management
- Safe staffing
- Nurse staffing levels: Impact of organizational characteristics
- In-patient midwifery staffing levels and postpartum readmissions
- Nurse staffing and outcomes in inpatient rehabilitation settings
- Appropriate staffing levels for US nursing homes
- Centers for Healthcare Strategies
- Staffing and Characteristics of Nursing Homes
- KFF: Five States with Toughest Nursing Home Staffing Rules Fail to Improve Care Quality












.png)

.png)
