Managing patient census can be one of the most complex tasks a facility faces.
Healthcare facilities face the daunting task of establishing adequate staffing levels without knowing the number of patients they will have on a given day.
Understaffing leads to poor health outcomes and staff dissatisfaction, while overstaffing is an inefficient use of resources and also leads to staff dissatisfaction.
Balancing staffing levels with a facility’s patient census is one of the most critical tasks healthcare administrators can achieve. This balance leads to:
- Improved patient care outcomes
- Staff satisfaction
- Efficient use of resources
Of course, the ultimate goal for any facility is to balance staffing levels with both patient census and acuity, to ensure that every patient receives the appropriate level of care.
What is patient census?
Patient census is the number of patients receiving care at a healthcare facility at a specific point in time. A patient census can include both inpatient and outpatient services, although it typically refers to the number of patients admitted to the facility for care.
Many facilities analyze patient census data to identify daily and weekly trends. Predictable factors that influence hospital patient census include the following:
- Nursing home schedules
- Work schedules
- Elective surgery scheduling
- Tendency to discharge patients around midday
Average census is calculated by taking the total number of patients for each day in a specific period. Some medical facilities calculate patient census once a day to measure the average daily census (ADC), while others calculate it hourly to collect more precise figures.
The average census is calculated by taking the total number of patients for each day in a specific period. For example, the average daily census is calculated by dividing the total number of patients each day over a given period by the number of days in that period.
Facilities often use data from previous years to predict patient census. An average census period refers to patient numbers that are comparable to those of the previous year.
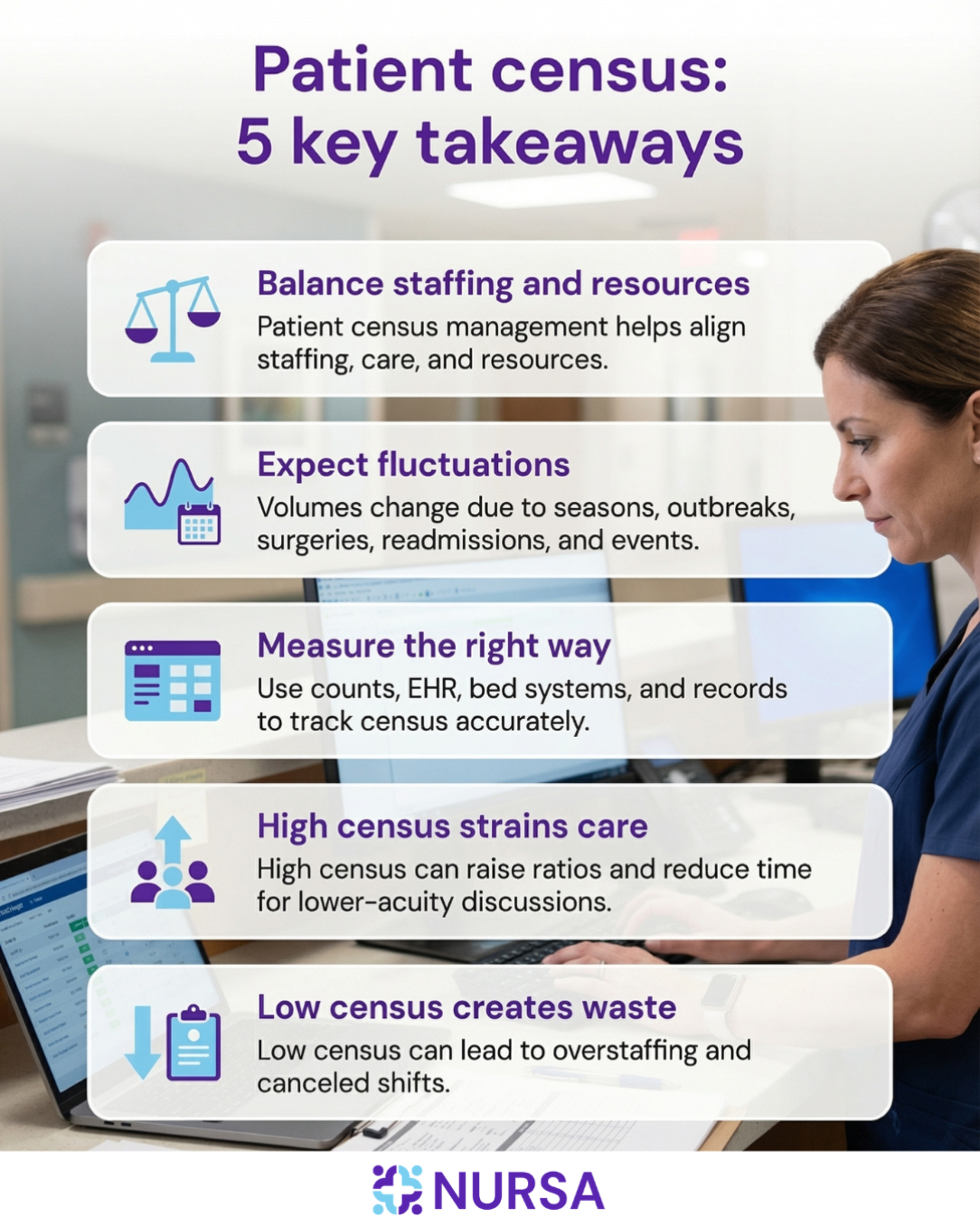
When patient numbers are significantly above average, there is a high patient census. When numbers are below average, there is a low patient census.
What causes fluctuations in the patient census?
Patient census fluctuations are driven by a variety of factors, some predictable and others completely unexpected. Identifying these factors is the key to effective census management:
- Seasonal patterns and trends: Seasonal illnesses, such as winter influenza or springtime allergy issues, often cause consistent patterns of peak patient volumes.
- Disease outbreaks: Sudden pandemics or single outbreaks of illness can create sudden and profound surges in demand for care.
- Elective surgeries: The scheduling of elective cases has a direct impact on patient census, as these patients occupy beds for a predetermined period of time.
- Readmissions: When a patient returns to the hospital shortly after discharge due to complications, it impacts the hospital's census.
- Other external events: Some events, like holidays, natural disasters, or accidents, can affect patient census.
How is patient census commonly measured?
Typically, healthcare facilities measure census using several methods to ensure they have an accurate picture of patient demand and, thus, their capacity.
Manual counts
Although manual, this is a common method that needs to be completed once or twice daily.
A designated staff member, often a supervising nurse, counts the admitted patients all at once at a specific time and records this information. This is used for calculating the average daily census.
Electronic health records (EHRs)
Modern facilities use their EHR systems, which track patient admissions, transfers, and discharges in real-time. This provides them with a dynamic, up-to-the-minute census, which is critical for making hourly bed-management and staffing decisions.
Some facilities are even implementing predictive analytics and machine learning tools that analyze a vast array of data (including weather, local school closures, and even social media sentiment) in addition to EHR data. This is a great addition as it provides a broader daily census forecast.
Bed management systems
Bed management systems are advanced systems that are connected to the EHRs. They provide a visual and functional representation of bed status across the facility.
These systems track occupied, unoccupied, and ready-to-clean beds, which directly impacts the effective census (the current number of patients a facility can admit).
Administrative records
For cost and long-term reporting, administrative and billing information are used to calculate the average length of stay and patient volumes by year, month, or week. Historical data is essential for strategic planning and budgeting.
High patient census
A high patient census means a hospital or medical facility is caring for a large number of patients. This typically results in higher nurse-to-patient and certified nursing assistant (CNA)-to-patient ratios, meaning each staff member must care for more patients simultaneously.
One concrete consequence of a high patient census is that rounding teams spend less time discussing essential topics related to the patient population, particularly those involving low-acuity patients.
Low patient census
A low patient census is when a facility has fewer patients to care for than normal. A low patient census can result in an overstaffed facility.
When this happens, clinicians may have their shifts canceled. Often, these cancellations affect their pay.
Some facilities have a budget to fund other projects during periods of low census. Thus, nurses can continue working and earning a salary despite a low census.
However, the policies on how to handle low census vary between facilities. Common practices include, for example:
- Asking the nurse to use their vacation time
- Sending the nurse home mid-shift
- Asking the nurse to be on call
As shown above, clinicians often bear the brunt of a low or decreasing patient census more than the patients or medical facilities themselves.
Why does the patient census matter?
Changes in patient census can affect facilities in aspects such as:
- Patient safety
- Health outcomes
- Resource capacity planning
- Use of overtime
They can also negatively impact morale and staff turnover rates. Therefore, healthcare facilities must accurately predict patient census and prepare for fluctuations in patient numbers.
The ultimate goal of monitoring the census is to inform staffing decisions for census purposes. Census management should be a primary strategic priority for schedulers and staffing managers, as it is often the leading driver of a wide range of operational decisions.
The following are aspects to consider regarding patient census and staffing in your facility.
Stay in compliance with nurse-to-patient ratios
Not all states mandate specific nurse-to-patient or CNA-to-patient staffing ratios. However, whether or not ratios are mandated, suboptimal staffing levels are detrimental.
- High nurse-to-patient ratios decrease the quality of care, patient safety, and patient satisfaction. There is evidence of increased adverse patient outcomes, including increased 30-day mortality and failure to rescue.
- High nurse-to-patient ratios also increase the risk of emotional exhaustion and job dissatisfaction among staff.
Improve how facility resources are allocated
Accurately predicting patient census can guide administrative and clinical decisions, such as bed management. Inaccurate predictions result in suboptimal staffing levels, whether that may be over- or understaffing. Facilities must predict patient census to provide safe patient care while using resources efficiently.
Improve budgeting and financial planning
By analyzing past and present data to make informed predictions, facilities can budget for the necessary resources to maintain adequate staffing levels. A staffing strategy that doesn’t take into account the patient census can result in a dramatic mismatch in a facility’s staffing levels and the amount of care needed to help its patient population.
Challenges in managing patient census
Managing patient census is no simple matter. Predicting and preparing for fluctuations in the patient census has long been a concern of hospital leaders.
Patient census not only affects staffing. It also has implications for hospital bed allocation and operating theater and radiology equipment run times. In short, it is intricately related to numerous aspects of a healthcare facility’s management.
The following are aspects that add to the complex nature of managing patient census:
Fluctuating demand for care
Facilities may be able to predict seasonal patient surges based on data from previous years. However, natural or manmade disasters are much harder to predict.
The COVID-19 pandemic is a prime example of unexpected increases in the demand for care. During the pandemic, there was a need to transition from staffing for regular volumes of patients to suddenly confronting an enormous and sustained surge of critically ill patients beyond existing census management paradigms.
Nurse staffing shortages
The ongoing nurse staffing shortage adds a layer of complexity to managing patient census. Due to the shortage, many facilities struggle to maintain adequate levels of internal staff.
The nursing shortage stems from numerous causes:
- An aging population requiring more care
- A large segment of the nursing workforce is reaching retirement age
- Limited resources to educate new nurses
- A significant percentage of nurses are leaving the profession
Nurse burnout
Nurse burnout is both a cause and a result of inadequate management of patient census.
A high patient census, combined with high nurse-to-patient ratios, can lead to nurse burnout. Burnout can lead nurses to leave their jobs and, in some cases, the profession altogether. In turn, this further contributes to the nursing shortage, which makes it difficult for facilities to maintain adequate staffing levels.
Patient satisfaction
Just as high patient census and high nurse-to-patient ratios lead to nurse burnout, they also lead to patient dissatisfaction. The higher the number of patients a nurse provides care for, the less time they have for each patient. This decreases the quality of care, patient safety, and patient satisfaction.
How to plan for and respond to a fluctuating patient census
Many facilities use the average census from the previous year or years to predict patient census. However, this approach alone does not offer facilities enough information to manage fluctuations in patient census adequately.
In addition to analyzing past data, the following census management strategies can help healthcare facilities plan for and manage fluctuating patient census.
1. Track average daily census (ADC) regularly
The average daily census is calculated by dividing the total number of inpatient days in a specific time period by the number of calendar days in that period.
The average daily census can help facilities adapt to current demands. For example, a hospital may notice that the ADC has been consistently higher than it was at the same time the previous year. In these cases, the fixed average census is no longer helpful, and facilities should base their predictions on current trends.
Furthermore, the time of day facilities calculate the ADC is crucial. Many calculate the average daily census at midnight. However, a study that analyzed hourly fluctuations in the ADC found that it peaked at 11:00 a.m. and was lowest at 7:00 p.m.
Understanding these hourly fluctuations can help facilities manage staff more effectively. Facilities should also consider calculating the ADC during higher patient census hours to guarantee sufficient staff throughout the day.
Pro-tip: To help you identify sustained changes in patient volume, your facility can calculate ADC monthly and compare it to the same month in the previous year.
2. Leverage technology to make data-driven decisions
Most hospitals now use electronic health records (EHRs). Access to each patient's status in real time can help facilities anticipate short-term changes in patient census.
EHRs enable facilities to track the current patient census at any given time and help them predict the patient census for the next 12 or 24 hours. By analyzing EHRs, facilities can predict when each patient will be ready for discharge.
Pro-tip: Use EHR data to generate daily discharge forecasts, allowing staffing managers to assign staff and make bed assignments for new patients in advance.
EHRs are vulnerable to cyber attacks. Keep your facility safe by implementing these tips to boost cybersecurity.
3. Reduce readmission rates
Another way to manage patient census is to reduce hospital readmission rates. Reducing readmission rates enhances patient outcomes and lowers healthcare costs. The following are crucial considerations for reducing readmissions:
- By improving the quality of care, hospitals can prevent unnecessary readmissions.
- Hospitals can guarantee a higher quality of care by maintaining adequate staffing ratios.
- Hospitals should also identify high-risk patients to prevent readmission.
- Healthcare staff must provide patients with sufficient education and comprehensive plans for care after discharge. This can include coordinating referrals for outpatient services or home health care and scheduling follow-up appointments.
Your facility can also implement transitional care management (TCM) protocols to make certain that high-risk patients receive complete follow-up phone calls and medication reconciliation within 48 hours of discharge.
Pro-tip: Ensure complete discharge planning before the patient leaves the facility. This includes scheduling outpatient services or home health referrals and follow-up appointments.
4. Lean on flexible, short-term staffing solutions
Managing nurse staffing is complicated, so hospitals need a variety of solutions. Long-term employees are essential, and travel nursing can be useful, though costly. However, for immediate staffing gaps, contracting PRN clinicians is the most efficient option.
- Baseline staffing: Nursa has found that high-performing facilities can strategically plan for census variability by staffing for the typical low-census periods or staffing for 80-90% of total facility capacity and incorporating layers of per diem staffing contingency as care demand increases. Facilities can also prepare for expected increases in patient census by posting PRN shifts days or weeks in advance.
- Maximize flexibility: By relying on contingency staff during periods of high patient census, facilities can maintain safe nurse-to-patient ratios. During periods of low patient census, facilities simply do not post PRN shifts and instead conserve their resources. This flexibility is a significant advantage over utilizing travel nurses since travel nursing contracts often protect nurses from shift cancellation.
5. Optimize patient length of stay
Facilities, especially hospitals, must understand and regulate the patient flow from admission through discharge.
- Control admissions and transfers: Hospitals can develop criteria for not admitting patients who will not benefit from the transfer. They can also postpone elective transfers during times of high patient census.
- Enable discharge: Social workers in the emergency department can help coordinate home services and simplify follow-up care, thereby avoiding unnecessary admissions.
- Use daily huddles: Physician-led daily census huddles can address expected patient census issues and help overloaded services improve bed turnover. The huddles can also reassign staff to address current needs.
Pro-tip: Start a "Target Discharge Date" for all admitted patients, updating and revising it daily in team huddles to proactively manage bed turnover.
6. Adopt staffing models suited to meeting census
To adapt to census changes, a facility needs to have a clear structure for its internal staffing. Staffing models should already incorporate census data and patients' needs.
Your facility can meet patient census more effectively depending on the model it uses:
Ratio-based staffing
A ratio-based model is the simplest, dictating a specific number of patients per nurse, regardless of patient complexity. It offers a minimum guaranteed level of staffing and is easy to implement and monitor. However, this model doesn’t consider the severity of the illness, which can lead to understaffing during times of high acuity.
Grid-based staffing
Grid-based staffing utilizes a grid or matrix that matches a specific census number with a predetermined number of staff for the shift. The advantages are that it establishes a clear, predictable budget and schedule plan. However, like with ratio-based staffing, it doesn’t account for patient acuity.
Acuity-based staffing
Acuity-based staffing is the most responsive model, where staffing is determined by the overall care hours required, which are based on the severity of illness and the dependency status of each patient (acuity). Although this is a model that optimizes patient outcomes, it requires more time and analysis to operationalize with a highly developed patient classification system.
Pro-tip: Incorporate a patient classification instrument to calculate daily or shift-by-shift acuity scores and determine the final staffing complement based on that score, varying the number of PRN shifts accordingly. Demand-based staffing might be the solution your facility needs.
7. Establish team workflows and policies to adapt to census changes
Effective census management requires effective communication and pre-determined institutional policies, such as:
- Daily team huddles: Conduct short, interdisciplinary huddles (physicians, nurses, social workers, administration) at the start of each shift or daily.
- Surge staffing protocols: Designate a plan for increasing capacity when high census is projected.
- Planning ahead for periods of reduced census: Have a non-punitive process for reduction in staffing during low census to minimize financial loss and prevent staff frustration when overstaffed.
- Avoid peak-chasing: Do not overstaff on a permanent basis, based on multiple historical high-census peaks. This leads to chronic overspending.
- Manage staff burnout: While on a low census, ensure that nurses who had been working high-census shifts are provided with adequate time off to recover.
Pro-tip: Conduct regular "post-surge" debriefings with staff to gain feedback regarding surge protocols and identify non-value-added activities that can be eliminated during times of high stress.
Seamlessly manage patient census with Nursa
Effective patient census management is an organizational culture shift from reactive crisis management to proactive resource planning. Facilities can have a resilient and patient-focused operating environment that provides both financial health and staff well-being when having access to:
- Real-time technology
- Patient acuity data
- Flexible staffing strategies and models
With Nursa, healthcare facilities can access vetted, qualified nurses to meet their short-term needs.
There's no need for facilities to make long-term commitments to PRN staff. They can simply post shifts when extra coverage is required, eliminating concerns about staff utilization during periods of low census.
Furthermore, this flexible staffing option helps facilities reduce overtime and avoid other costs associated with understaffing.
Adapt to a fluctuating patient census by contracting PRN staff to meet your facility’s changing needs. Post the PRN shifts you need to fill today.
Sources:
- National Library of Medicine: Time Series Analysis for Forecasting Hospital Census: Application to the Neonatal Intensive Care Unit
- National Library of Medicine: Practical development and operationalization of a 12-hour hospital census prediction algorithm
- National Library of Medicine: Effects of Unit Census and Patient Acuity Levels on Discussions During Patient Rounds
- National Library of Medicine: Finding the time: Hourly variation in average daily census on a hospital medicine service
- Lippincott Nursing Center: AJN Report: The Other Side of Mandatory Overtime
- HealthManagement: New approach for hospital census management












.png)

.png)
