Cancer in women’s reproductive organs can be life-changing—but early detection and surgical care save lives every day. Discover how gynecologic oncologists combine precision, teamwork, and compassion to guide patients from diagnosis through recovery.
Gynecologic oncology: A guide to surgical treatment and cancer care
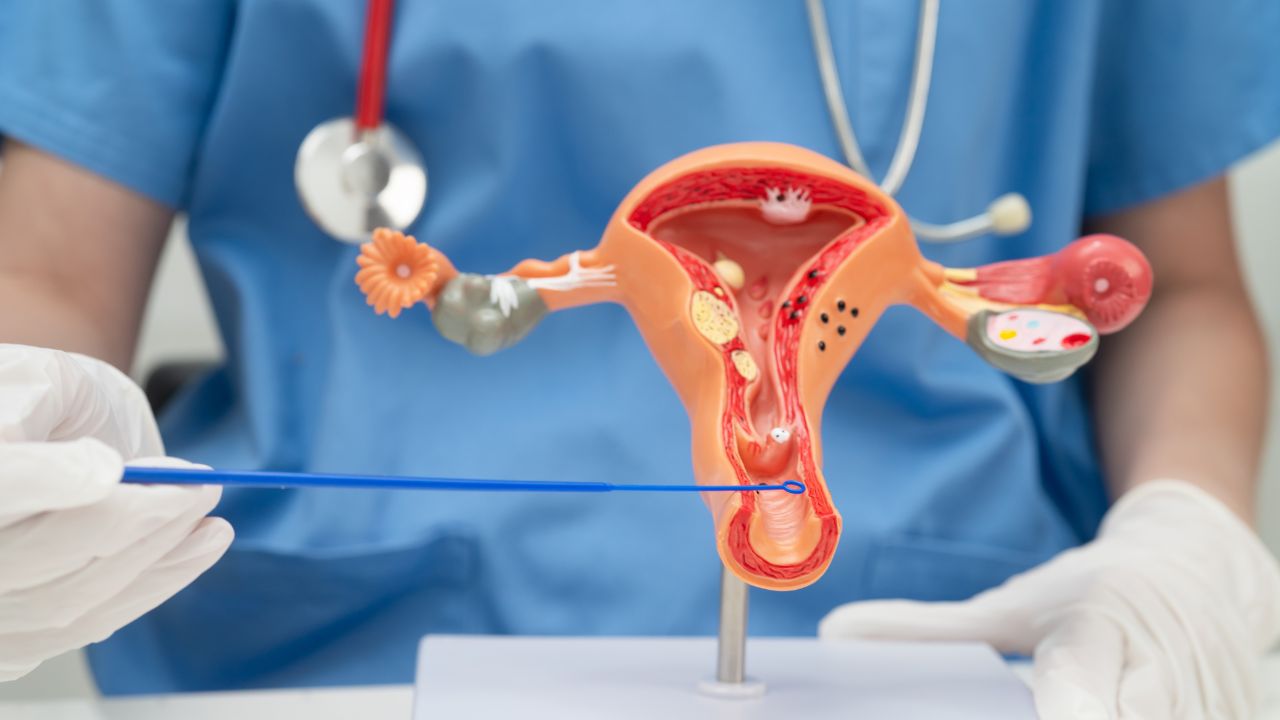
Gynecologic oncology focuses on the surgical treatment and management of cancers that affect the female reproductive system. These include cancers of the uterus, cervix, ovaries, fallopian tubes, vulva, and vagina.
This field combines surgical precision with compassionate, multidisciplinary care—helping women navigate diagnosis, treatment, and recovery with the goal of restoring health and quality of life.
Understanding gynecologic oncology
Gynecologic oncology is a specialized branch of medicine that addresses cancers of the reproductive organs.
Unlike general gynecologic surgery, which may treat conditions like fibroids or endometriosis, gynecologic oncology involves procedures to diagnose, stage, and remove cancer, often as part of a broader plan that includes chemotherapy, radiation therapy, or immunotherapy.
Early detection and surgical intervention remain central to improving survival rates. Each procedure is guided by the type of cancer, its stage, and the patient’s overall health, fertility goals, and preferences.
What does a gynecologic oncologist do?
A gynecologic oncologist is a surgeon with advanced training in both obstetrics-gynecology and oncology. They provide comprehensive cancer care that spans from diagnosis to treatment and follow-up.
Their role includes:
- Performing biopsies and staging surgeries to determine how far cancer has spread
- Removing tumors and affected tissue with precision
- Collaborating with medical oncologists, radiation oncologists, and pathologists to coordinate care
- Offering fertility-preserving surgical options when medically appropriate
These specialists often manage complex cases requiring a delicate balance between cancer control and maintaining hormonal, sexual, and reproductive health.
Types of gynecologic oncology surgeries
Gynecologic oncology surgery encompasses a range of procedures tailored to each cancer type and its progression. While some operations are minimally invasive, others require open or combined approaches for complete tumor removal and staging.
Diagnostic and staging procedures
- Biopsy: Removal of a small tissue sample for microscopic analysis to confirm malignancy.
- Laparoscopy: A minimally invasive method that allows visual inspection of the pelvic and abdominal organs to detect metastasis.
- Lymph node dissection: Sampling or removal of lymph nodes to determine if cancer has spread.
- Surgical staging: Determines the extent of disease and helps plan follow-up therapies.
Therapeutic surgeries
- Hysterectomy: Removal of the uterus, often used for endometrial or cervical cancer. Depending on the case, it may be partial, total, or radical (including nearby tissue and lymph nodes).
- Oophorectomy and salpingectomy: Removal of the ovaries or fallopian tubes, often indicated for ovarian or fallopian tube cancer.
- Debulking surgery: In advanced ovarian cancer, the surgeon removes as much of the visible tumor as possible to enhance the effectiveness of chemotherapy.
- Radical vulvectomy or trachelectomy: Procedures that remove cancer from the vulva or cervix while preserving surrounding healthy tissue when feasible.
- Fertility-sparing surgery: Selective removal of tumors in early-stage cancers to preserve reproductive potential under oncologist supervision.
Minimally invasive and robotic-assisted approaches
Modern gynecologic oncology increasingly relies on minimally invasive surgery, including laparoscopy and robotic-assisted techniques. These approaches reduce trauma, blood loss, and recovery time while providing excellent visibility for surgeons working in the confined pelvic space.
Laparoscopic oncology surgery
Surgeons operate through tiny incisions using a camera and fine instruments to perform biopsies, hysterectomies, or staging procedures. This technique allows faster recovery and shorter hospital stays.
Robotic-assisted surgery
Robotic systems provide magnified 3D views and allow high-precision movements that mimic a surgeon’s hands. They’re especially valuable in complex pelvic surgeries, such as radical hysterectomy for cervical cancer or lymph node removal near vital structures.
Why minimally invasive matters
For eligible patients, minimally invasive gynecologic oncology surgery means:
- Reduced pain and shorter hospitalization
- Lower risk of infection and scarring
- Faster recovery and return to daily life
- Improved cosmetic and emotional outcomes
While open surgery is still necessary for certain advanced or bulky cancers, minimally invasive options continue to expand, reflecting progress toward precision and preservation in cancer care.
The multidisciplinary oncology team
Effective gynecologic oncology care depends on teamwork. From diagnosis to recovery, specialists collaborate to ensure every aspect of a patient’s treatment plan is integrated and compassionate.
A typical gynecologic oncology team includes:
- Gynecologic oncologist: Leads surgical and treatment decisions.
- Medical oncologist: Manages chemotherapy or targeted drug therapies.
- Radiation oncologist: Plans and administers radiation therapy when indicated.
- Anesthesiologists and perioperative nurses: Ensure surgical safety and patient comfort.
- Pathologists and radiologists: Analyze tissue and imaging to guide treatment.
- Nurse navigators, social workers, and physical therapists: Provide support for recovery, education, and emotional well-being.
This collaborative model ensures that no step in cancer care happens in isolation—each decision is informed by a full view of the patient’s medical, physical, and emotional needs.
Preparing for gynecologic oncology surgery
Preparation for gynecologic oncology surgery involves both medical and emotional readiness. The process helps ensure safety, reduce anxiety, and improve recovery outcomes.
Preoperative evaluation
- Comprehensive review of medical history and imaging
- Blood work, ECG, and anesthesia assessment
- Discussion of fertility preservation or menopausal implications
- Review of medications, smoking, or alcohol use that could affect healing
Patient education and consent
Patients receive clear explanations of the surgical plan, potential risks, and postoperative expectations. This stage often includes consultations with oncology nurses and fertility specialists.
Emotional and logistical preparation
- Counseling or support groups for coping with a cancer diagnosis
- Planning for home recovery, transportation, and caregiver support
- Guidance on nutrition, physical activity, and pre-surgery fasting
A well-prepared patient is better equipped to manage recovery and recognize early signs of complications.
Postoperative care and recovery
Recovery after gynecologic oncology surgery varies based on the type of procedure, the patient’s overall health, and whether additional therapies are planned.
Immediate recovery
- Monitoring of vital signs, urine output, and incision sites
- Pain management using multimodal analgesia
- Prevention of complications such as infection or blood clots
Early home recovery
- Gradual return to activity with rest periods
- Wound care and hygiene instructions
- Awareness of warning signs such as fever, swelling, or unusual discharge
Long-term recovery and follow-up
- Regular oncology follow-ups to monitor healing and detect recurrence
- Pelvic rest until cleared by the surgeon
- Nutritional support and physical therapy to rebuild strength
- Counseling for body image or emotional adjustment
Comprehensive recovery extends beyond immediate recovery in the post-anesthesia care unit or even physical healing—it includes emotional and psychological adaptation to life after cancer surgery.
Subspecialties within gynecologic oncology
While all gynecologic oncologists address reproductive cancers, each cancer type presents unique surgical and treatment challenges.
- Ovarian cancer surgery: Often involves tumor debulking, omentectomy, and lymph node dissection.
- Endometrial (uterine) cancer surgery: Commonly managed with hysterectomy and staging to guide further therapy.
- Cervical cancer surgery: May include cone biopsy, trachelectomy, or radical hysterectomy depending on stage.
- Vulvar and vaginal cancer surgery: Requires delicate excision to maintain urinary and sexual function while ensuring complete tumor removal.
- Fertility-sparing oncology surgery: For early-stage cervical or ovarian cancers, specific techniques preserve reproductive potential under careful follow-up.
Each subspecialty underscores the goal of combining effective cancer control with respect for quality of life.
Technology and innovation in gynecologic oncology
Advances in technology continue to reshape gynecologic oncology, bringing greater accuracy, safety, and personalization to surgical cancer care.
Imaging and visualization
High-definition and fluorescence-guided imaging help surgeons identify lymph nodes and cancer margins more precisely. Near-infrared technology enhances the visibility of blood vessels, reducing complications.
Energy-based and hemostatic tools
Modern instruments allow controlled cutting and coagulation, reducing blood loss during complex oncologic procedures such as radical hysterectomy or lymphadenectomy.
Digital pathology and AI
Artificial intelligence assists in rapid tissue analysis, helping pathologists confirm margin status during surgery and supporting real-time decision-making.
Personalized surgical planning
3D modeling and simulation tools enable tailored approaches based on each patient’s anatomy and tumor characteristics. These tools help oncologists plan fertility-sparing or reconstructive steps in advance.
Integration with reproductive technology
Collaboration between oncologists and fertility specialists allows ovarian tissue cryopreservation, egg freezing, and other options before cancer treatment begins—expanding choices for younger patients.
Beyond the operating room: The impact of gynecologic oncology
Gynecologic oncology represents more than a surgical discipline—it’s a holistic commitment to women’s health, dignity, and survivorship.
Every procedure, from tumor removal to reconstruction, reflects the blend of science, precision, and compassion that defines modern cancer care.
Through early detection, advanced technology, and coordinated teamwork, gynecologic oncologists strive not only to treat cancer but to help women reclaim their sense of wholeness and confidence after diagnosis.